Uses and Limitations of Pulse Oximetry
Pulse oximetry is often overlooked as an unimportant stat to record for a patient’s overall health. But one of the first things a physician will ask for in a medical emergency is the oxygen saturation of the blood. Knowing the blood oxygen levels helps physicians understand what a patient’s overall physical state is and address their condition the best way possible. Prior to 1980, the pulse oximeter was not available for regular use. If a physician needed to know the blood gas level, they had to perform an arterial blood gas test, or ABG, which is a blood draw taken from the radial artery in the wrist. This procedure is particularly uncomfortable for the patient as the artery is deep in the wrist. Additionally, a physician would have to wait to get the results, which then delayed treatment that may be desperately needed.
The first noninvasive pulse oximeter became available for use in 1981, after being invented in the early 1970s. Initially, these devices were only used to monitor patients that were under anesthesia or heavy sedation. After extensive research, they discovered that pulse oximeters could detect hypoxemia, or abnormally low blood oxygen levels, and prevent a significant number of deaths that occurred under anesthesia. After this discovery, pulse oximeter usage expanded to emergency departments and eventually to medical offices. Now, pulse oximetry is considered vital information when evaluating a patient’s overall health.
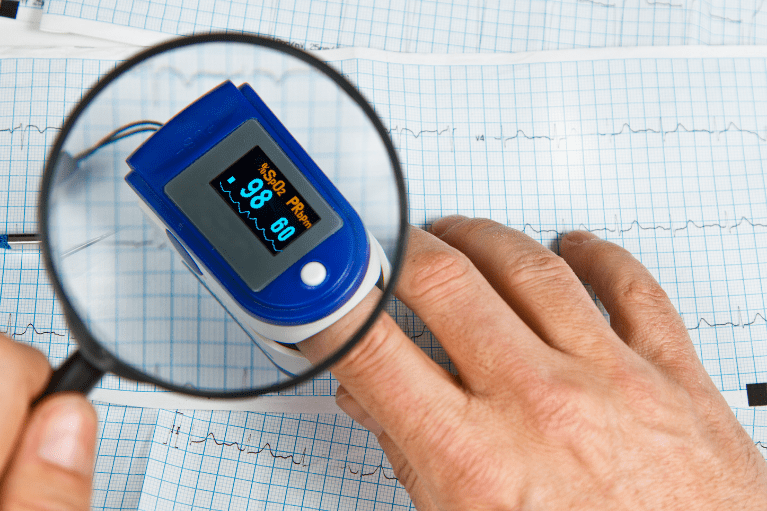
What Does a Pulse Oximeter Do?
Pulse oximetry measures the blood’s oxygen saturation, that is, how much oxygen is circulating throughout the body at a given time. When we breathe oxygen into the lungs, it binds to a protein called hemoglobin in a red blood cell. The blood becomes oxygenated and circulates throughout the body, via the arteries, to deliver oxygen to the organs, tissues, and cells to use as fuel. An adequate amount of oxygen is needed for the organs to function properly and keep our bodies working accordingly. If not, vital organs will start to fail. Once the tissues use up the oxygen, it is converted to carbon dioxide. The red blood cells bind to the carbon dioxide and return to the lungs through the veins to be exhaled.
How Does it Work?
3+
Pulse oximetry works by detecting the amount of oxygen bound to red blood cells at a given time. A pulse oximeter clamps onto the tip of a finger or wherever the skin is more transparent, such as an earlobe or toe. The device emits an infrared light that shines through the smallest blood vessels to the other side of the device. A sensor detects the amount of light absorbed by the oxygenated red blood cells and gives a percentage of red blood cells loaded with oxygen. Readings of 95%-100% are within normal limits, and anything below 90% is considered abnormal and indicates a condition called hypoxemia. Blood oxygen levels below 90% may be caused by an underlying medical condition that requires medical intervention with certain medications or supplemental oxygen.
Watching oxygen saturation levels is particularly useful for individuals that suffer from conditions that affect breathing and blood oxygen levels, including conditions such as COPD, pneumonia, or sleep apnea. It is also useful in measuring how well the heart is pumping blood throughout the body. Individuals with conditions like anemia, congenital heart defects, or heart failure may have an adequate amount of oxygen in their lungs, but the cardiovascular system does not function efficiently enough to deliver it to the rest of the body. When this occurs, it can result in hypoxia, meaning the tissues are depleted of oxygen.
Uses of Pulse Oximetry Include:
- Monitor patients under anesthesia or sedation to alert medical staff of any fluctuations in blood oxygen level.
- Determine the need for supplemental oxygen.
- Determine whether someone has significant drops in oxygen levels while asleep, which could suggest possible sleep apnea.
- Evaluate ability to handle increased physical activity.
- Monitor known respiratory conditions and the effectiveness of current oxygen therapy treatment.
Limitations of Pulse Oximetry:
While pulse oximeters are extremely useful, quick, and easy to use, there are some situations that can impede the device’s ability to produce accurate readings. It is essential that the device has a good signal, so readings are not falsely high or low, but sometimes this is difficult to obtain. Pulse oximeters get their readings from the pulsation of blood through the arteries. So, if a patient has a heart condition, is dehydrated, or is critically ill causing a weak pulse, the oximeter readings will be inaccurate, or the device may not be able to generate anything at all.
Additionally, the device may be placed incorrectly, have an improper fit, or get knocked out of place from movement or a sleeping position change. Excessive movement in the form of seizures, shivering, tremors, or wiggling can impede the device’s ability to pick up a signal, and therefore it cannot generate a reading. If the pulse oximeter does not fit correctly, it will not detect the pulse or give significantly low, inaccurate numbers. If the oximeter is too big, it will slide around on the finger, and if the device is too small, it can cut off circulation. Therefore a proper fit is necessary. There may also be difficultly generating readings in cold environments, in rooms with bright lights due to sensor interference, and in patients wearing dark nail polish.
In some instances, pulse oximeters may give normal readings when actually there is not an adequate amount of oxygen circulating throughout the body. This occurs in cases of carbon monoxide poisoning. The protein hemoglobin binds to carbon monoxide more readily than oxygen. Therefore, if hemoglobin has already bound with carbon monoxide over oxygen, the pulse oximeter will give a falsely elevated reading. In these cases, an ABG test would be necessary to diagnose and treat carbon monoxide poisoning effectively. The same is true in individuals with anemia. Anemia is a condition in which the red blood cells do not have a sufficient amount of hemoglobin. So, the circulating red blood cells will be carrying all the oxygen they can hold; however, the organs are not receiving the necessary amount of oxygen, causing the tissues to suffer and potentially become hypoxic. Finally, pulse oximetry is not an indication of ventilation. Therefore individuals with respiratory failure and decreased breathing rate can have normal pulse oximeter readings but may not be eliminating carbon dioxide from the body properly.
Final Thoughts
While pulse oximetry has come a long way in medicine, there are still situations in which a more invasive ABG test is necessary. And although some limitations can hinder the results from a pulse oximeter, it is still the quickest, noninvasive way to alert physicians of an underlying medical condition, or severity of a current illness, so that they can provide care as quickly as possible to their patients.