Cardiac Arrhythmias Guide: Types, Symptoms, and Diagnosis
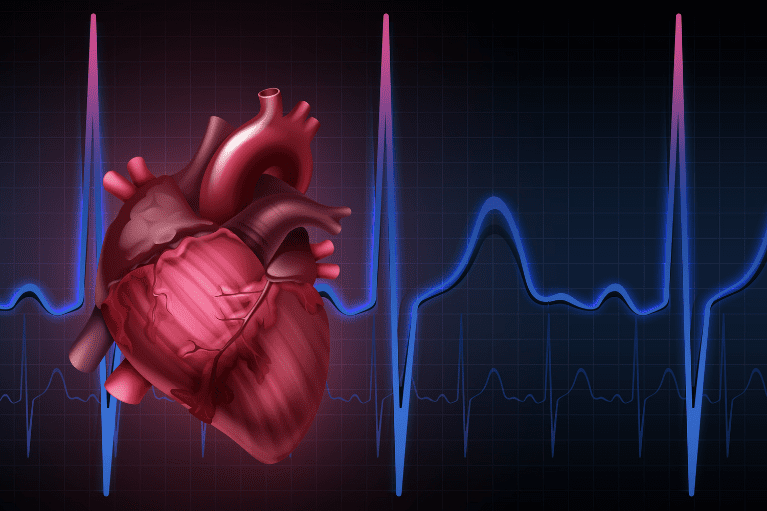
Cardiac arrhythmias refer to conditions where the heart beats too fast, too slow, or in an irregular pattern. When this occurs, the heart does not function efficiently, decreasing the amount of blood being pumped throughout the body. Arrhythmias develop due to changes in heart tissue, activity, or electrical signal that controls the heartbeat. Sometimes, when these events occur, it can be so brief that the overall heart rate is not affected and therefore unnoticeable. However, some arrhythmias can be severe and cause dizziness, fainting, and difficulty breathing, as well as an increased risk of having a stroke or going into cardiac arrest. Here is everything you need to know about cardiac arrhythmias.
What Causes Cardiac Arrhythmias?
Several factors can affect the electrical impulses within the heart and interrupt a normal rhythm. Even individuals with a healthy heart can experience an arrhythmia from time to time, but will hardly experience a long-term arrhythmia from an isolated event. Underlying conditions that can increase the risk of cardiac arrhythmias include heart attack, scarring of heart tissue, high blood pressure, coronary artery disease, cardiomyopathy, heart valve disorders, hyperthyroidism/hypothyroidism, electrolyte imbalances, diabetes, and sleep apnea. Other lifestyle choices that increase the chance of cardiac arrhythmias are excessive alcohol or caffeine consumption, drug abuse, smoking, stress, anxiety, certain medications, and supplements.
There are Different Types of Cardiac Arrhythmias
The heart has four chambers, two atria, and two ventricles, in which cardiac arrhythmias can originate. The atria sit above the ventricles. If an arrhythmia originates in either atrium, it is called a supraventricular arrhythmia. If they arise from either ventricle, it is called a ventricular arrhythmia. Arrhythmias are also classified by the effect on resting heart rate. Typically, in healthy individuals, the heart will beat 60 to 100 times a minute. If it beats less than 60 times a minute, it is called bradycardia and more than 100 times a minute is tachycardia.
Examples of Supraventricular Arrhythmias:
- Premature atrial contractions – early or extra beating of the atrium.
- Atrial fibrillation – irregular quivering of the atria causing increased heart rate; this is the most common type of arrhythmia.
- Atrial flutter – similar to atrial fibrillation in which the atria are not contracting correctly, but in a more consistent rhythm.
- Supraventricular tachycardia (SVT) – rapid heart rate that stays in a regular rhythm.
- Accessory pathway tachycardias – extra electrical pathways increasing impulses that cause the heart to beat unusually fast.
- AV nodal re-entrant tachycardia (AVNRT) – Fast heart rhythm caused by an extra electrical pathway through the AV node.
Examples of Ventricular Arrhythmias:
- Premature ventricular contractions – early or extra beating of the ventricles; among the most common type of arrhythmias.
- Ventricular tachycardia – rapid premature beating that does not allow the ventricles to completely fill with blood. This can be a more serious type of arrhythmia because the heart is not pumping an appropriate amount of blood.
- Ventricular fibrillation – disorganized quivering of the ventricles. V-fib is life-threatening and requires immediate medical intervention.
- Long QT syndrome- Ventricles take too long to contract and release.
Bradyarrhythmias, or arrhythmias that cause a slow heart rate, are another type of arrhythmia that occurs due to a problem with the conduction system, such as sinus node dysfunction, heart block, or certain medications. Sinus node dysfunction causes a slow heart rate because of an abnormality in the SA node that delays sending signals that initiate a contraction. Heart block is a delay or complete obstruction of the electrical impulses initiating contractions, resulting in an irregular, slow rhythm.
Symptoms
Symptoms of cardiac arrhythmias differ from person to person and vary depending on the type of arrhythmia. Cardiac arrhythmias may not produce any symptoms, and your doctor may be able to notice it before you do. Some common symptoms associated with tachycardia are shortness of breath, dizziness, fainting, rapid pulse, feeling a “skipped” beat, chest pain, lightheadedness, and sudden weakness. Bradycardia can have similar symptoms. However, symptoms typically associated with bradycardia are fatigue, abundant sweating, dizziness, confusion, fainting, shortness of breath, difficulty breathing, cardiac arrest, and death.
Diagnosis
Before a physician runs any test, they will perform a thorough exam that includes obtaining a family history of any heart conditions or heart problems that have caused sudden death. They will then detect any possible risk factors for cardiac arrhythmias. It is important to discuss specific symptoms you have experienced so the proper tests can be performed. Oftentimes, cardiac arrhythmias cause a mismatch between pulse and heart rhythm, so it is important that these are monitored during an evaluation. Because arrhythmias can come and go, there are a few tests a physician can use to detect the type of arrhythmia. The first is an electrocardiogram (EKG), which records the electrical activity of the heart. Another kind of EKG is a Holter monitor. This device is a portable EKG worn at all times, except showering, for one to two days. An event monitor is another way to track heart activity over a period of time. Event monitors are recommended for detecting cardiac events that do not happen regularly. When symptoms arise, the individual must push a button to start recording to catch the event. Typically, the monitor is worn for a month or longer. If necessary, a physician may recommend a more permanent option like an implantable loop recorder. This device is placed under the skin and continuously records the heart’s electrical activity. Other tests include a stress test that detects how much stress the heart can tolerate, an echocardiogram, cardiac catheterization, electrophysiology study, and a head-up tilt table test that can determine the cause of fainting spells.
Next steps
After diagnosing a cardiac arrhythmia, the next step is to figure out how to treat it. Treatment depends on the type of arrhythmia and the severity of the condition. Most of the time, treatment is not necessary at all. For bradycardia, the best treatment option is a pacemaker, as long as there is no underlying cause for the slow heart rate. A pacemaker is a device placed under the skin in the chest or abdomen that regulates heart rate by sending electrical pulses to initiate a beat and maintain a regular heart rate. Tachycardia has several options to help keep heart rate within normal ranges. Treatment options include medication, lifestyle changes, invasive therapies, electrical devices, and surgery.
Some examples of treatments for tachycardia are:
- Vagal maneuvers like coughing, holding your breath, and dunking your head in ice water to return heart rate to normal.
- Medications are useful in reducing the number of episodes and can help electrical conduction of the heart.
- Cardioversion, or shocking, is an electrical shock delivered through paddles on the chest to correct the electrical impulses and return the heart to a normal rhythm. This is useful in atrial fibrillation cases.
- Catheter ablation is a procedure where a catheter is placed through a blood vessel into the heart and creates a block in the pathway causing the arrhythmia.
- Implantable cardioverter-defibrillator is a device that is placed in the chest and monitors heart rate, and if the heart rhythm is off, the device sends shocks to restore normal rhythm.
- Maze procedure is a surgical procedure where a cut is made in the heart to form a scar that will block electrical impulses to help the heart beat correctly.
- Ventricular aneurysm surgery is a surgical procedure that removes a bulge in the blood vessel leading to the heart that can cause an arrhythmia.
- Coronary bypass surgery is a procedure that improves blood supply to the heart by placing a graft from an artery or vein onto the coronary artery to evade a blockage.
Prevention
The long-term outlook for cardiac arrhythmias depends on the type and any underlying causes that increase overall health risk. Serious arrhythmias like ventricular fibrillation need immediate medical intervention as death can occur very quickly. With the advancements of medicine and devices that regulate heart rate, the prognosis has improved for serious arrhythmias. While some arrhythmias are not preventable, certain measures can be taken to ensure heart health, so more severe conditions do not develop. Regular checkups with your physician are beneficial to prevent medical conditions that can lead to cardiac arrhythmias. Lifestyle changes including eating a healthy, well-balanced diet, keeping cholesterol and blood pressure under control, not smoking, exercising regularly, maintaining a healthy weight, managing stress, and finally limiting alcohol and caffeine consumption are also recommended for reducing the risk of cardiac events,
As always, consult your physician if you believe you could be at risk or think you are experiencing cardiac arrhythmias.